
Interprofessionality as part of the solution to the lack of skilled workers
Oct. 2021Interprofessionality and coordinated care
Between 2017 and 2020 the FOPH implemented a support programme to promote interprofessional education and cooperation. This issue of spectra looks at the findings and recommendations that have emerged from four years of research and practical implementation – and at the way forward.
“Interprofessional education is a tool. It’s a tool to accomplish linkages between the education system and the health care delivery system. It is a tool to achieve better patient care. It is a tool to achieve better health for the public. It is a tool to achieve a more efficient and affordable health care system.”
George E. Thibault, Institute for Medicine of the National Academies (USA)
The support programme “Interprofessionality in healthcare 2017–2012” originated from the skilled workers initiative. The question then (as now) was: How can we maintain our healthcare system so that it continues to meet needs in the future in the face of the impending lack of skilled workers? The answer is as follows: What is needed is healthcare that focuses even more intently on patients. At the same time, better use must be made of the potential for increasing efficiency.
Interprofessional collaboration (IPC) makes an important contribution on both counts. Studies indicate that IPC has a direct influence on the quality of care because it is aligned with patients’ needs and optimises coordination between the different healthcare professionals. It also has an indirect impact on the quality of care as a result of greater job satisfaction among the professionals because interprofessional teams work more on an equal footing instead of operating within rigid hierarchies. This means that skilled workers stay in their profession for longer, which in turn has a positive effect on the continuity of care and thus on the quality of the services provided. But IPC also helps to increase efficiency within the healthcare system because, if professionals work in a coordinated manner and as one unit, it is easier to avoid duplication.
Support programme approved
The Federal Council approved a budget of CHF 3 million for a support programme implemented between 2017 and 2020 to enable the Swiss healthcare system to benefit from IPC. The programme focused not only on research (e.g. to improve the scientific basis of care) but also on practical aspects (e.g. the compilation of good-practice models) and generated a wide variety of results. A total of 18 research projects were funded. They included a cost-benefit analysis of interprofessional collaboration and a study of the potential of interprofessional education. Although the programme produced some fascinating findings, it is difficult to derive definitive answers because a patient’s well-being or successful teamwork in a hospital depends on a large number of other factors in addition to good IPC. So, for example, there is no final answer to the question of whether IPC is less expensive overall. While costs do not appear to be an obstacle – at least in the inpatient setting – the results do show that the rate of staff fluctuation is lower in interprofessional teams.
In the second area, practical implementation, the main aim of the support programme was to increase the visibility of good-practice models and networking between the different players. At the start of the programme, the FOPH called on interested professionals to present models exemplifying the successful implementation of interprofessional education (IPE) and IPC in the everyday medical setting. Interest was so great that a directory providing profiles of the models, activities and tools was created on the FOPH website. It now has nearly 80 entries. The directory will be continued beyond the end of the research programme so that it can continue to provide stakeholders interested in interprofessionality with ideas in the future. Some of these models were portrayed in depth in two publications. They show how collaboration between different professionals (and beyond) can succeed and how IPE is lived out.
Four policy briefs
Another important outcome of the programme was the four policy briefs for the areas of inpatient and outpatient care, the psychiatric-somatic interface, and training. Each policy brief summarises the major findings from four years of research and the recommendations that can be derived from them. “It was important for us that these recommendations were developed jointly with the stakeholders and can now provide guidance or a basis for the next steps,” explains Cinzia Zeltner, a member of the scientific staff at the FOPH and the project lead.
“Whether in a hospital, a doctor’s practice, an old people’s home or a nursing home, IPE and IPC must be both practised and promoted by management.”
Yet, after four years of the support programme, one question remains to be answered: what is now needed to establish IPC more firmly in the healthcare system? One major factor in ensuring success here is initial and continuing training and professional development. Healthcare professionals need to learn early on how to interact with other professions. They must learn to speak a common language, develop a common stance and recognise the problems at the interfaces. “All healthcare professionals consequently need to be taught this subject while they are training,” explains Lara De Simone-Nalotto, a scientific project assistant at the FOPH. Things have certainly changed for the better in this respect over the past few years, but it will take years, if not decades, for the change to have an effect in practice. In the context of life-long learning, IPE needs to become an integral element of continuing training and professional development so that collective skills are developed continuously (e.g. during in-service training).
Leadership also plays an important role because progress is only possible if leaders are willing to drive interprofessionality. Whether in a hospital, a doctor’s practice, an old people’s home or a nursing home, IPE and IPC must be both practised and promoted by management. This is the only way in which interprofessionality can succeed in the everyday work situation. It is clear that this topic will continue to play an important role in the future – the impending shortage of skilled workers will be a problem in the Swiss healthcare system for many years to come, and the results of the support programme show that successfully implemented IPC can help to mitigate the problem.
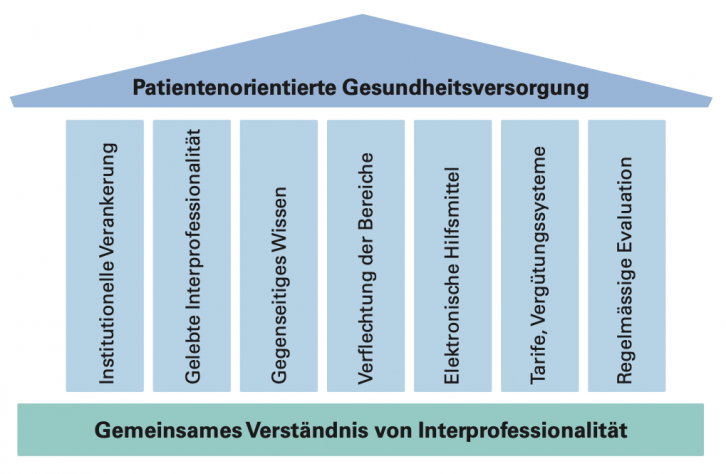
In den Forschungsprojekten des Förderprogramms konnten sieben gemeinsame Themenstränge identifiziert werden, welche alle auf dem Fundament des gemeinsamen Verständnisses von Interprofessionalität aufbauen mit dem Ziel, die Versorgung patientenorientierter zu gestalten.
Highlights des Förderprogramms 2017–2020
Die Ergebnisse des Förderprogramms bieten Bund, Kantonen, Gemeinden, Berufs- und Bildungsorganisationen sowie Leistungserbringern Instrumente, um die Interprofessionalität im Gesundheitswesen weiter zu stärken.
Forschungsprojekt
Insgesamt wurden 18 Forschungsprojekte finanziert, 3 aus dem Bereich Bildung, 15 aus dem Bereich Berufsausübung. Die dadurch erarbeiteten Erkenntnisse zu interprofessioneller Bildung und Zusammenarbeit dienen als Basis für die Erarbeitung praxisrelevanter Massnahmen.
Onlineverzeichnis
Modelle guter Praxis
Das Verzeichnis enthält Steckbriefe von Modellen guter Praxis mit dem Ziel, die Sichtbarkeit und Vernetzung der in der Schweiz tätigen Akteure zu fördern. Das Verzeichnis bleibt auch nach Ende des Förderprogramms bestehen und ermöglicht Interessierten, Modelle nach verschiedenen Kriterien wie Kanton, Interventionsbereich, Beruf, Setting etc. gezielt zu suchen. Interessierte können Modelle, Initiativen oder Aktivitäten im Bereich der Interprofessionalität einfach und schnell selbstständig eintragen. Der Eintrag kann auf Deutsch, Französisch oder Englisch erfolgen. Das BAG übernimmt die Übersetzung in die anderen Sprachen.
Publikationen
Im Rahmen des Förderprogramms publizierte das BAG zwei Broschüren, die anhand erfolgreicher Beispiele zeigen, wie gelebte Interprofessionalität aussehen kann, wo die Herausforderungen liegen und welche Chancen sich bieten. Die beiden Broschüren (erhältlich auf Deutsch, Französisch und Italienisch) richten sich in erster Linie an die lokalen, regionalen und kantonalen Leistungserbringer bzw. Bildungsanbieter im Gesundheitswesen.
Im Rahmen der Forschungsprojekte wurden zudem Broschüren zur frühzeitigen Intervention bei Kindern und Jugendlichen zur Förderung der psychischen Gesundheit sowie ein Leitfaden für Gesundheitsfachpersonen im Bereich widersprüchliche Einschätzungen publiziert.
Tool zur Erfassung der Interprofessionalität
Wie interprofessionell ist unsere Institution unterwegs? Mit dem «Schweizerischen Interprofessionalitäts-Evaluationsinstrument» (kurz: SIPEI) kann in einer Institution der Ist-Zustand erörtert werden. Das Tool umfasst Fragebögen für die Stufen Mitarbeitende, Vorgesetzte sowie Patientinnen und Patienten und kann sowohl zur Selbstevaluation als auch zur Fremdevaluation angewendet werden (erhältlich auf Deutsch, Französisch und Italienisch). Kontaktperson: .
Vier Policy Briefs
Die wichtigsten Erkenntnisse, die im Rahmen des Förderprogramms gewonnen wurden, wurden in vier Policy Briefs bereichsspezifisch zusammengetragen. Ziel dieser Dokumente ist, den politischen Entscheidungsträgern, Berufsorganisationen, Bildungsverantwortlichen sowie Leistungserbringern eine kurze und knappe Übersicht über bestehende Herausforderungen und mögliche Lösungsansätze zu geben.
Veranstaltungen
Zwei grosse Veranstaltungen wurden durchgeführt: 2018 organisierten das BAG, die Schweizerische Akademie der Medizinischen Wissenschaften (SAMW) und die Plattform Interprofessionalität die gemeinsame Tagung «Interprofessionalität im Gesundheitswesen: Better Chronic Care» im Berner Kursaal. Im November 2021 fand die Schlusstagung des Förderprogramms «Interprofessionalität im Gesundheitswesen» statt.




